Seismocardiography for Primary Care (pocket-guide)
A practical visual guide to SCG waveforms and what they may suggest
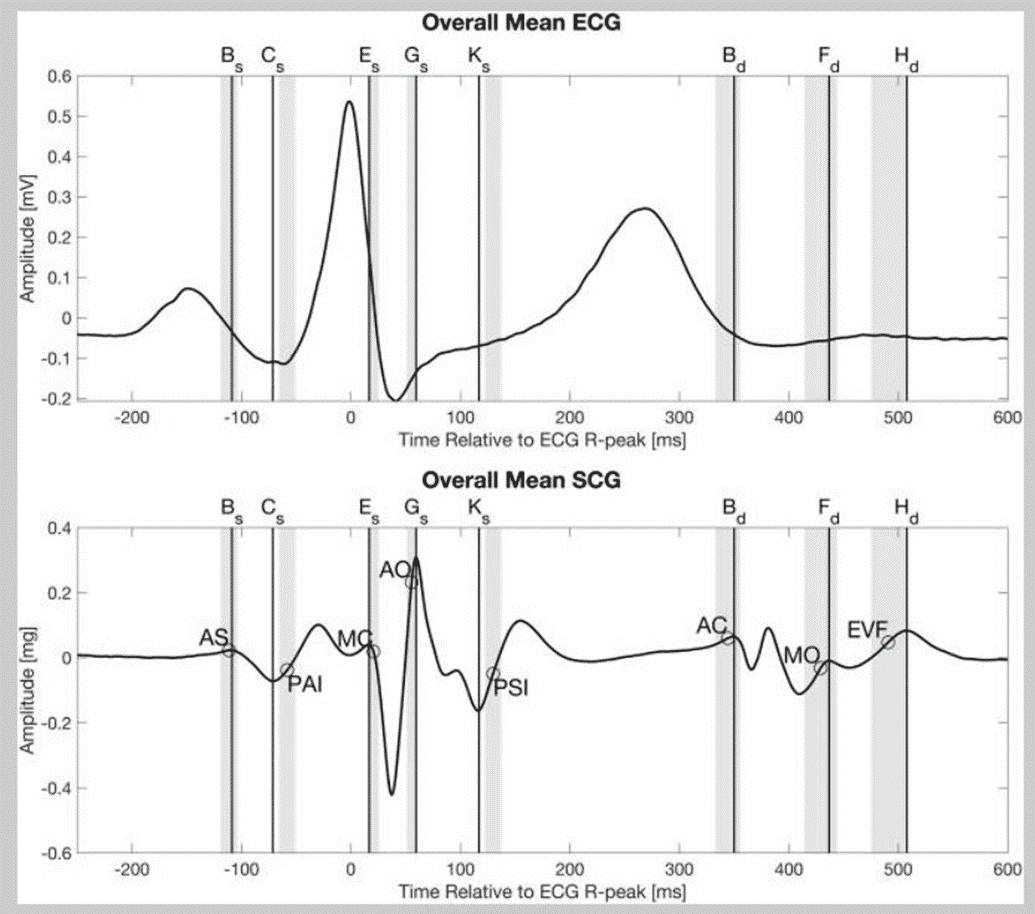
What SCG measures
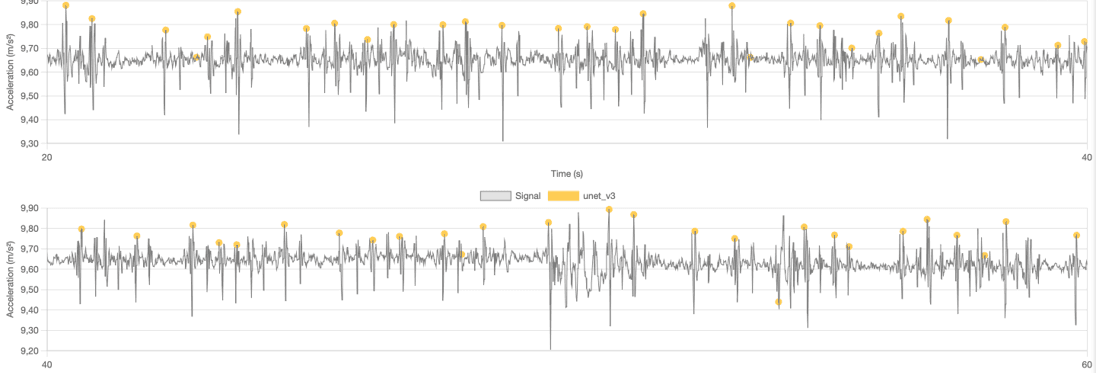
- SCG is a chest vibration signal from cardiac mechanics recorded by an accelerometer.
- In routine traces you usually see two dominant systolic landmarks:
- AO - aortic valve opening, the main ejection “thump.”
- AC - aortic valve closure, the second prominent peak.
- Timing tracks ECG rhythm: mechanical events follow the electrical R wave by a short electromechanical delay. You read SCG the same way you read a pulse strip: rate, regularity, and beat-to-beat strength.
Acquisition basics that matter
- Phone or sensor on the chest with firm contact. Two useful spots: mid-sternum or left lower ribs near the apex.

- 60-120 s recording, minimal movement, normal breathing. Note coughs, sighs, or posture changes.
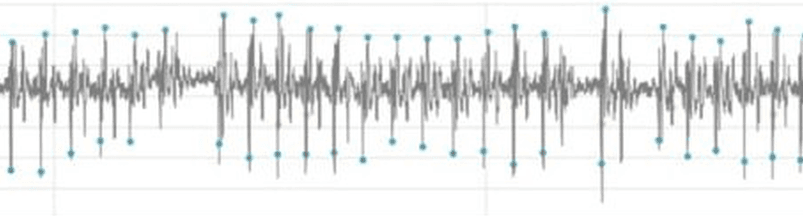
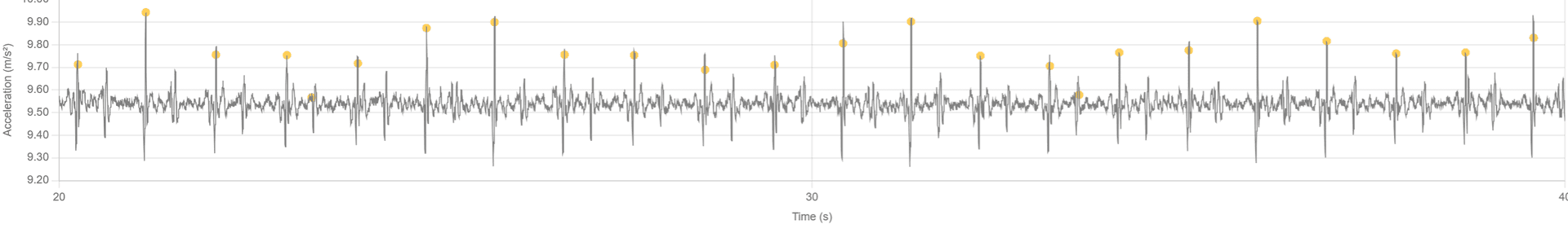
How to read an SCG quickly
- Rate and regularity - are intervals even or not.
- Amplitude - does AO height stay stable or alternate.
- AO-AC timing - is the systolic interval stable or drifting.
- Pauses - any long gap, and what happens after it.
Visual patterns you can trust
Below, related patterns are grouped. For each group: what you see, how to tell look-alikes apart, and what it may suggest. This is pattern recognition, not a diagnosis.
Group 1 - Early beats and pauses
PAC vs PVC on sight
- Shared visual core - an early beat with smaller AO than neighbors.
- PAC hint - the following pause is shorter than a full compensatory pause. Rhythm feels “nudged,” then snaps back.
- PVC hints
- Beat can be smaller OR paradoxically larger/deformed compared to neighbors.
- Compensatory pause longer – often looks like a whole cycle missing.
- The next AO is larger (postextrasystolic potentiation).
- Patient often describes: “thump → pause → strong thump.”

- Clinical idea - PAC is supraventricular, PVC is ventricular. This split is useful triage, but ECG decides.
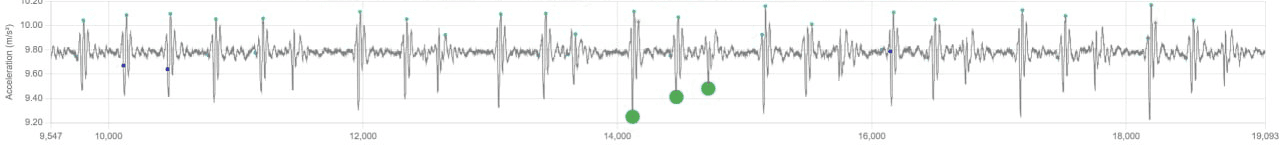
Postextrasystolic potentiation
- What you see - after a longer pause, the next AO is clearly taller.
- Meaning - more filling, stronger beat. Common after a PVC. Not a diagnosis on its own, but confirms the pause was real.
Sinus pause / SA exit block
- What you see - a single long flat gap with no SCG peaks, then the old rhythm resumes at the same rate.
- How to separate from AV block - in AV block you may see periodic dropped mechanical beats forming a repeating group pattern. A lone long gap that resets cleanly suggests sinus pause.
- Meaning - missed sinus impulse or exit block. Note duration and symptoms.
Group 2 - Alternating strong and weak beats
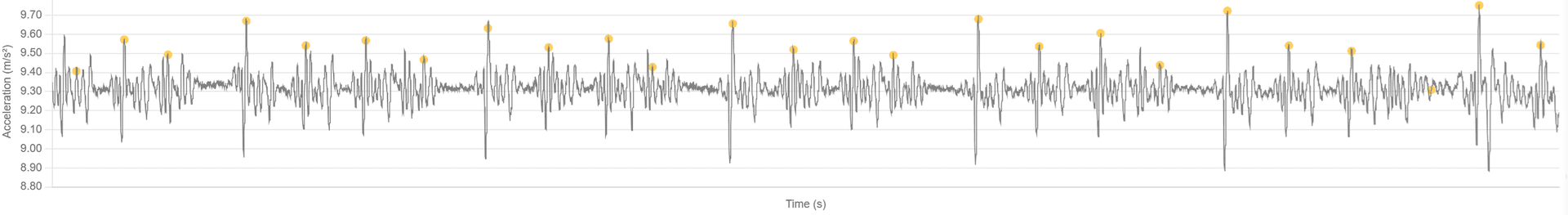
Bigeminy / trigeminy vs pulsus alternans
- Bigeminy - strict alternation strong–weak–strong–weak with regular timing. Often the weak beat is an ectopic with a shorter coupling interval. Can present as 2 normal + 1 weak (trigeminy).
- Pulsus alternans - alternation of AO height at a steady rate without obvious premature coupling. Looks like strong–weak–strong–weak with equal spacing.
- Quick split
- If every weak beat is early and followed by a longer pause → think bigeminy.
- If timing stays even and only amplitude alternates → think pulsus alternans.
- Meaning
- Bigeminy - ectopy in a regular pattern.
- Pulsus alternans - reduced contractile reserve, consider LV dysfunction context.
Group 3 - Regular fast runs
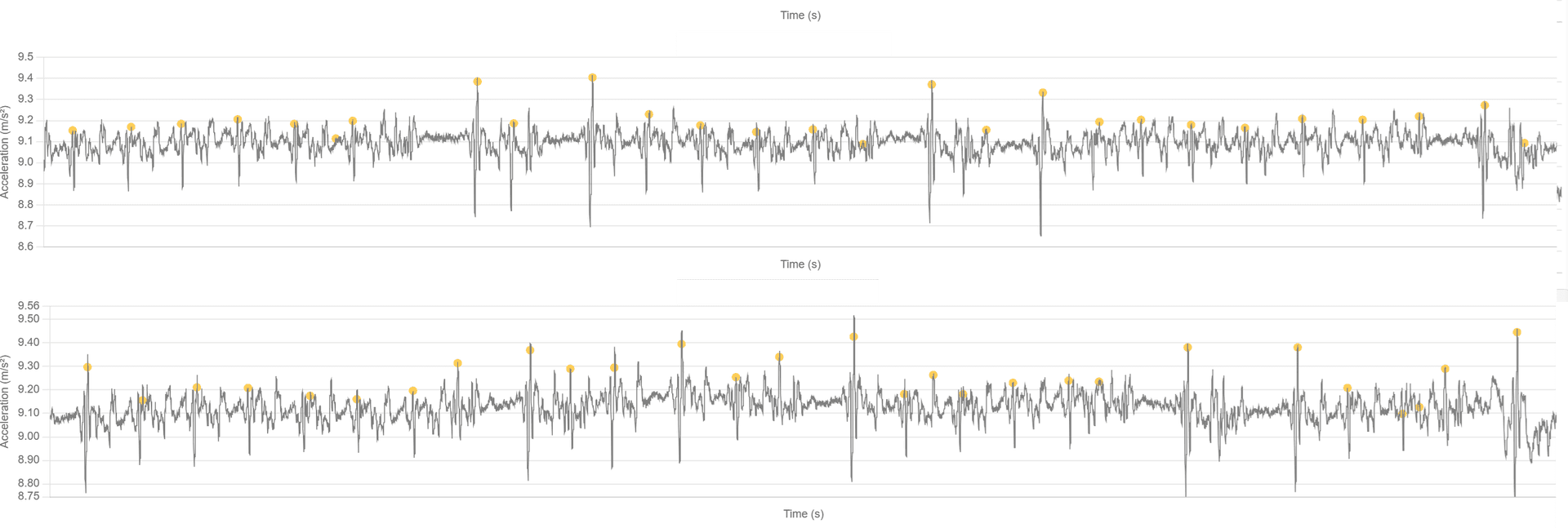
Sinus tachycardia vs short monomorphic SVT (PSVT)
- Shared - a block of densely packed, similar-amplitude beats.
- Sinus tachycardia - gradual speed-up and slow-down, amplitude tracks physiology. Usually context driven (stress, exertion, fever).
- PSVT - abrupt start and abrupt stop, rate is very regular and often faster than typical sinus. Appears as a compact burst then clean return to baseline.
- Meaning - sinus is expected response, PSVT is a paroxysm worth documenting and correlating with symptoms.
Group 4 - Irregular rhythms
Atrial fibrillation
- What you see - irregularly irregular intervals and variable AO heights beat to beat. No repeating cadence.
- How to separate from artifact - AF keeps a pulse cadence despite variability. Motion artifact creates noncardiac deflections and off-rhythm chunks.
- Meaning - AF pattern on SCG is a red flag for ECG confirmation and risk assessment.
Group 5 - AV conduction phenomena
Wenckebach (Mobitz I) vs Mobitz II vs AV dissociation
- Wenckebach (Mobitz I)
- What you see - a grouped pattern: cycles where AO-AC timing or beat spacing drifts, culminating in a dropped mechanical beat, then the group repeats.
- Meaning - progressive conduction delay with periodic non-conducted beat.
- Mobitz II
- What you see - mostly stable timing with intermittent dropped beats without preceding drift. Example 2:1 or 3:1 mechanical pattern.
- Meaning - higher-grade block. Red flag for escalation.
- AV dissociation
- What you see - AO-AC relationship is unstable. The systolic interval wanders, AC can appear “out of place,” and large beats may show up at odd times as atria and ventricles march independently.
- Meaning - complete AV block or ventricular rhythm. Urgent ECG correlation.
Group 6 - Sinus bradycardia with periodic pauses
- What you see - slow, regular sequence with occasional longer gaps, AO height otherwise stable.
- Meaning - often physiologic during sleep or in trained individuals. Context and symptoms decide if this is benign or needs ECG.
Group 7 - Respiratory modulation
- Physiologic respiratory sinus arrhythmia
- What you see - cyclic small changes in intervals and AO height in phase with breathing.
- Possible pulsus paradoxus
- What you see - consistent AO reduction on inspiration that is larger than usual and repeats with each breath.
- Caution - strong respiratory effects are a clue, not a diagnosis. Correlate with clinical picture and blood pressure if concerned.
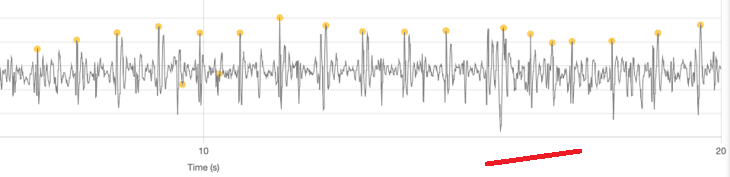
Pitfalls that masquerade as pathology
- Motion and posture - turning the torso, talking, coughing, chuckling. These inject noncardiac wiggles. Real beats keep a coherent cadence.
- Contact and pressure - loose sensor or changing hand pressure flattens AO randomly across several seconds. True alternans keeps a beat-to-beat pattern.
- Breath holds and sighs - a big sigh can look like a pause plus amplified next beat. Check for concurrent respiratory deflection.
- Orientation - SCG amplitude can vary with angle. Rate and the presence or absence of a beat are more reliable than raw height.
Minimal workflow a non-cardiologist can follow
- Scan 60–120 s with good contact and quiet breathing.
- Mark the cadence - regular, grouped, irregularly irregular, or fast bursts.
- Inspect AO height dynamics - stable, alternating, intermittently weak, post-pause boosted.
- Map to this guide and write a plain hypothesis:
- Early small beat + long pause + big next beat → likely PVC with compensatory pause and postextrasystolic potentiation.
- Strict alternation at even timing → likely pulsus alternans.
- Grouped pattern ending in a missed beat → likely Wenckebach.
- Irregularly irregular intervals with variable heights → likely AF.
- Abrupt fast burst → likely PSVT run.
- Lone long gap with clean resumption → likely sinus pause.
- Unstable AO-AC relationship and odd “big beats” → possible AV dissociation.
When to escalate
- Syncope, chest pain, dyspnea, or presyncope with any abnormal pattern.
- Suspected Mobitz II, AV dissociation, sustained fast tachycardia, or AF in a new patient.
- Frequent PVCs in runs or bigeminy with symptoms.
Final notes
- SCG is a mechanical lens on rhythm. It is excellent for spotting patterns you can also feel at the wrist.
- Use SCG to form a working hypothesis and to time ECG capture or referral.
- Document context: symptoms, activity, medications, and any triggers during the recording.